- Home
- Alcohol Related Liver Disease (ALD)
Alcohol Related Liver Disease (ALD)
Alcohol Related Liver Disease (ALD)
At a glance
- ALD is a condition where the liver is damaged over time by alcohol
- The disease typically has three stages
- Abstinence from alcohol in the first stage – fatty liver – can result in liver healing
- Click here to read Amanda’s story with ALD
What is it?
Alcohol-related liver disease (ALD) is a condition where the liver is damaged over time by alcohol. Alcohol is broken-down by the liver. This process results in harmful chemicals which can damage and kill liver cells. Although the human liver is very resilient to damage, its ability to recover from regular alcohol consumption and the breakdown process becomes unsustainable. This can cause scarring which can eventually lead to cirrhosis, typically in three stages which include fatty liver, alcohol-related hepatitis or inflammation and alcohol-related cirrhosis.
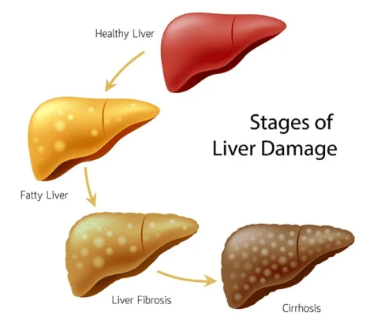
Fatty liver may be revealed by an abdominal ultrasound, in the absence of symptoms. If alcohol abstinence occurs at this point, and for a prolonged period of time (months to years) the liver can heal itself and recover.
Alcohol-related hepatitis is the second stage which occurs after years of harmful drinking and particularly following a sudden increase in drinking. It can develop suddenly, typically with jaundice appearing over weeks. It is a very serious condition which can lead to liver failure or death.
Alcohol-related cirrhosis is the most advanced stage of alcohol-related liver disease (ALD) and infers that liver scarring is now irreversible. Up to 1 in 5 heavy drinkers will develop liver cirrhosis. If one gives up alcohol entirely at this point, the liver can still work to sustain normal life, providing it has not decompensated and there is an absence of ascites, jaundice or internal bleeding. Appropriate screening and monitoring are vital at this point.
Liver cirrhosis is associated with an increased risk of liver cancer and, consequently, 6-monthly scans of the liver should be undertaken to screen for cancer. If detected at an early stage, liver cancer is curable.
Diagnosis
ALD is generally diagnosed by blood tests and scans in those with a history of alcohol excess. Liver blood tests may demonstrate signs of liver damage with elevated gamma GT or AST (liver enzyme). A number of scanning techniques can also diagnose ALD including ultrasound and transient elastography such as FibroScanTM). Endoscopy or OGD may be used to identify enlarged veins (varices) in the oesophagus and stomach. A liver biopsy might also be undertaken to examine liver tissue microscopically and diagnose the nature and extent of liver damage.
Treatment / management
The main goals of management are to achieve abstinence from alcohol and maintaining this habit.
In addition to alcohol abstinence, an individual with ALD can prevent further liver damage by maintaining a healthy weight, managing any pre-existing conditions such as type 2 diabetes and liver conditions such as haemochromatosis or hepatitis C. Women are more vulnerable to the harms of alcohol than men and some alcohol-related diseases appear to be genetic.
There are medications such as campral and vivitrol for those struggling to achieve abstinence from alcohol. In those who develop acute alcohol-related hepatitis medication to reduce liver inflammation, such as steroids, may be required.
Other medications may be used to indirectly support the liver such as beta-blockers; used in liver disease to reduce the pressures in the veins related to the liver. Alcohol-related liver disease is one of the leading conditions for which liver transplants are performed in Ireland. The criteria for liver transplantation are quite strict, given the relative size of the donor pool in contrast to demand.
Prognosis
Management of ALD and alcohol cessation is the mainstay of treatment and prevention.
