Budd Chiari Syndrome
Liver Illness
At a glance
-
Budd Chiari syndrome describes a blockage or narrowing in the hepatic vein, the outflow from the liver
-
A blockage can be caused by a blood clot (thrombus), a malignant or benign tumour or membranous webs
-
The syndrome is so called after Dr George Budd and Dr Hans Chiari, who both described hepatic venous outflow obstruction
- Click here to read Karol’s story with Budd Chiari Syndrome
What is it?
Budd Chiari syndrome (BCS) is a rare disorder where the vessel draining blood from the liver, the hepatic vein, becomes narrowed or completely blocked. This results in an accumulation of blood in the liver cells (hepatocytes) which causes liver injury or damage or, on occasion, liver failure. It can be experienced as acute, subacute or chronic forms, inferring that an individual can be under treatment for BCS for sometime, or it may present as a sudden or acute occurrence, resulting in a medical emergency.
Primary and secondary BCS refer to an obstruction within and outside of the hepatic vein(s), respectively. Primary BCS is more commonly thrombotic (caused by a blood clot or thrombus) but non-thrombotic blockages might include ‘membranous’ or ‘caval’ webs. Compression of the 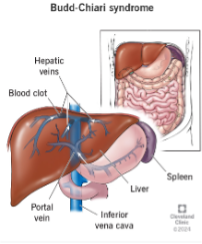 hepatic vein by outside pressures, secondary BCS, might also halt or disrupt blood draining from the liver. Pressure on or damage to the hepatic vein can be caused by liver tumours, cysts, abscesses or from chemotherapy, infections or trauma.
hepatic vein by outside pressures, secondary BCS, might also halt or disrupt blood draining from the liver. Pressure on or damage to the hepatic vein can be caused by liver tumours, cysts, abscesses or from chemotherapy, infections or trauma.
Most commonly, the underlying cause is a disorder where blood clots occur, including some chronic blood cancers, pregnancy, sickle cell disease or contraceptive pills.
Typical symptoms
Symptoms of Budd Chiari syndrome are similar to those of other liver disease or damage and include jaundice, itching, extreme fatigue and lethargy, abdominal distension or swelling known as ascites, loss of appetite and nausea. One may also have right shoulder pain.
Clinical presentation
A person with Budd Chiari syndrome may present with elevated LFTs (liver function tests), an increase in liver enzymes in the blood. They might be nauseous and drowsy, and an abdominal examination might reveal ascites (an accumulation of fluid in the abdominal cavity). There may also be hepatomegaly (enlargement of the liver), and splenomegaly (enlargement of the spleen). Portal hypertension (pressure buildup in the portal vein carrying blood from the digestive tract and spleen to the liver) and varices may also be observed. Varices are varicose veins of the oesophagus, stomach or rectum, which, in some instances, can rupture.
Diagnosis
The gold standard in diagnosis of BCS is by scanning techniques such as ultrasound and / or MRI (magnetic resonance imaging), when other liver diseases have been eliminated.
Incidence
Budd Chiari syndrome is an uncommon disorder, affecting just one in 100,000 of the general population. It appears to affect men and women equally, typically between the ages of 20 and 40. Geographically, membranous or caval webs appear to be more common in southeast Asia and the Middle East than in the western world.
 Treatment
Treatment
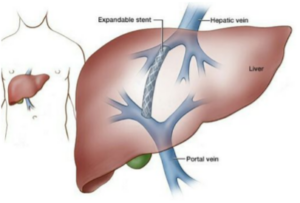
Treatment options are dependent on the presentation and whether it is an acute or chronic form, but the treatment aim will always focus on eliminating the blockage or compression and restoring the blood flow from the liver. Transjugular intrahepatic portosystemic shunt (TIPS) refers to a procedure where a bypass of the hepatic vein is created. This technique describes the connection of the portal vein (the vein that carries blood to your liver) to one of the hepatic veins with a stent (tiny metal tube). In addition, should the blockage be thrombotic, anticoagulation therapy or blood thinners such as heparin or warfarin might be administered to dissolve the blood clot. Other treatments might include minor surgical procedures to eliminate an external pressure or compression, removing a malignant or benign tumour, for example.
Prognosis
A person’s prognosis depends on various factors, including how severe the condition is and the individual’s response to treatment. In the absence of treatment, most people with a completely blocked hepatic vein die of liver failure within three to five years. A liver transplant may be the only viable option to prolong one’s life. Research shows people usually live longer if their veins are only partially blocked or narrowed.